Contact Us
Contact Us
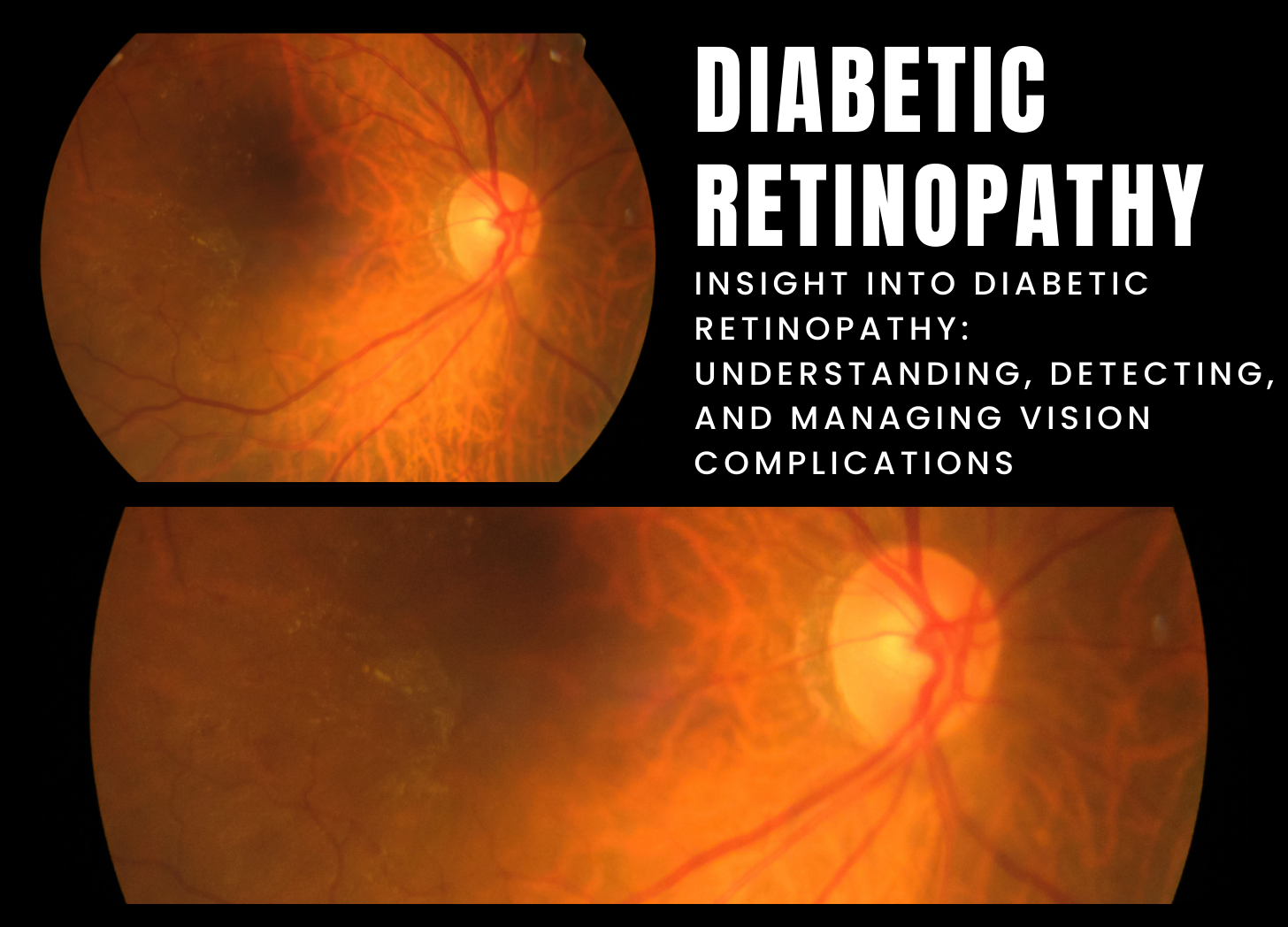
Diabetic retinopathy is a significant eye disorder that affects diabetics and is a major cause of vision loss and blindness. Long-term high blood sugar levels cause damage to the blood vessels in the retina, the light-sensitive tissue in the back of the eye. Diabetic retinopathy can affect people with type 1 and type 2 diabetes, and it usually develops gradually, advancing from mild to severe.
The specific etiology of diabetic retinopathy is unknown, although it is thought to result from damage to the retina’s tiny blood capillaries caused by prolonged exposure to high glucose levels in the blood. Over time, this damage can cause blood and fluid to seep into the retina, enlargement of the macula (the center region of the retina important for sharp, central vision), and the formation of aberrant blood vessels on the retina’s surface. These alterations can impair eyesight and, if left unchecked, cause permanent vision loss.
Common diabetic retinopathy symptoms include blurred or distorted vision, problems seeing colors, floaters (spots or dark strings floating in the field of vision), dark or empty patches in the vision, and fluctuating eyesight. Diabetic retinopathy may not generate apparent symptoms in its early stages, emphasizing the significance of regular eye exams for diabetics to detect and monitor retinal abnormalities.
Diabetic retinopathy is often diagnosed with a full eye examination that includes dilated eye exams, visual acuity tests, and retinal imaging (such as fundus photography or optical coherence tomography [OCT]) to study the retina’s structure and function. Diabetic retinopathy should be detected and treated early to preserve eyesight and avoid additional retinal damage.
Treatment for diabetic retinopathy is determined by the stage and severity of the condition, and may include lifestyle changes such as strict control of blood sugar, blood pressure, and cholesterol levels to limit disease progression. In mild to severe diabetic retinopathy, laser therapy (photocoagulation) or intravitreal injections of anti-vascular endothelial growth factor (anti-VEGF) drugs may be used to seal leaking blood vessels, shrink aberrant blood vessels, or minimize macula edema. In severe cases of diabetic retinopathy, surgical procedures like as vitrectomy (the removal of the vitreous gel) may be required to remove blood or scar tissue from the retina and enhance vision.
To summarize, diabetic retinopathy is a sight-threatening consequence of diabetes caused by damage to the blood vessels in the retina, which can lead to vision loss and blindness if not treated. Individuals with diabetes require regular eye exams, early detection, and adequate therapy of diabetic retinopathy in order to preserve vision and maintain eye health.
References:
1.American Academy of Ophthalmology. (2022). Diabetic Retinopathy. Retrieved from https://www.aao.org/eye-health/diseases/diabetic-retinopathy
2.National Eye Institute. (2022). Diabetic Retinopathy. Retrieved from https://www.nei.nih.gov/learn-about-eye-health/eye-conditions-and-diseases/diabetic-retinopathy
Post a Comment